01. Some cancers do run in families!
Everyone has a chance of developing cancer in their lifetime, but some people have an increased risk due to familial cancer genes.
A 2020 study from the Mayo Clinic published in the prestigious American oncology journal JAMA Oncology found a link between cancer and genetics. After genetic testing of 2,984 cancer patients, researchers found that 13.3% had heritable mutations in cancer-prone genes.
In 2016, JAMA published another study by Harvard University scientists and researchers from Denmark and Finland, which indicated that at least 22 types of cancer carry a high heritable risk. If a parent or sibling has had cancer in a family, the risk of other family members developing the same cancer increases by 33%.
It is important to note that "hereditary" here does not refer to directly inheriting cancer, but rather to inheriting a susceptibility to cancer. As a multi-gene genetic susceptibility disease, this is also a key factor in the clustering of tumors.
People with a family history of these five cancers are particularly at high genetic risk and must take preventative measures:
1) Breast Cancer
Breast cancer has a high familial risk. Studies have found that if a first-degree relative has breast cancer, the risk of developing the cancer themselves is 2-3 times higher than the average person. People with BRCA1 and BRCA2 gene mutations have the highest risk of breast and ovarian cancer.

2) Gastric Cancer
Having a first-degree relative with gastric cancer may also increase one's own risk. One of the rare hereditary forms of gastric cancer that should be considered is primarily caused by a CDH1 gene mutation. It is more common in young people and has a poor prognosis, so screening is essential.
3) Nasopharyngeal Cancer
Nasopharyngeal cancer also has a familial predisposition and can cluster in certain areas. It is primarily caused by the Epstein-Barr virus, especially in families where the disease is frequently transmitted through saliva, which can easily increase the risk of cancer.
4) Lung Cancer
Data indicates that lung cancer incidence is twice as high in those with a family history of cancer. Among patients with squamous cell lung cancer, 37.8% have a family history of the disease; among female patients with alveolar cell lung cancer, the rate is as high as 58.3%.
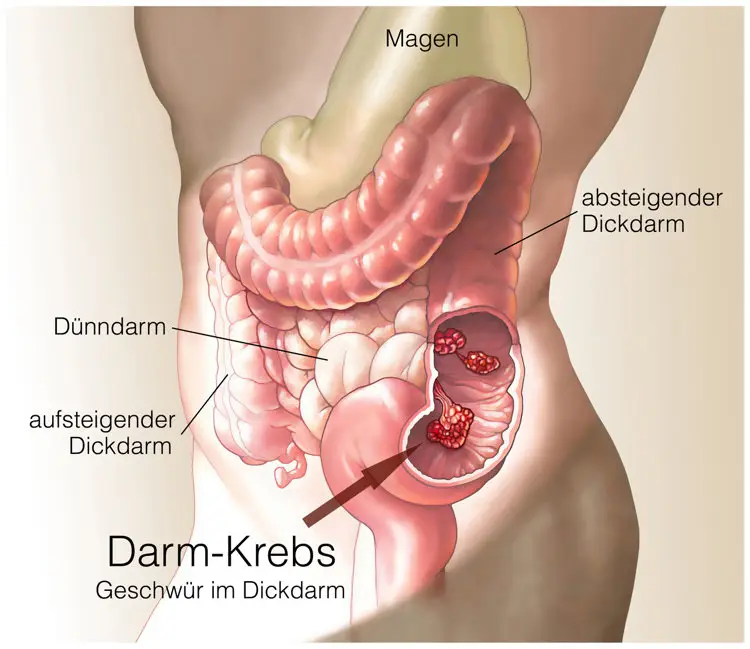
5) Colorectal Cancer
Many colorectal cancer patients have a history of intestinal polyps in their early years. While the development of intestinal polyps can be caused by many factors, including the autosomal dominant genetic risk factor of familial adenomatous polyposis (FANP), carrying this gene significantly increases the risk of developing the disease. Generally, children of parents with colorectal cancer and FANP have a 50% chance of inheriting the disease.
02. Cancer Heredity: Focus on Four Key Indicators
Although there is a certain risk of cancer running in families, this risk is not guaranteed. In reality, factors that contribute to cancer development include not only genetics but also diet, lifestyle, and psychological factors. A family predisposition to cancer should only be considered if the following characteristics are present.
1) Multiple
Three or more family members have developed the same or related cancer. For example, cancers related to the BRCA gene include breast, ovarian, pancreatic, and prostate cancers. Although they occur in different organs, they are all related cancers.
Also, if the same patient develops two cancers, or cancers in paired organs, such as bilateral breast cancer or ovarian cancer, or if two or more lesions occur in the same organ, a genetic risk should be highly suspected.

2) Early Onset
If a family member has a history of cancer, pay attention to the age of onset. Generally, the earlier the age of onset, especially around 30 years old, the more likely it is a significant indicator of genetic predisposition.
3) Rare
Rare refers primarily to a relatively uncommon type of cancer, such as breast cancer in a male family member.
4) Related Genes
If you're tested for tumor genes, such as the common BRCA1/2 genes, which are high-risk genes for breast and ovarian cancer, the risk of breast cancer in Asians is as high as 56%, and the incidence of ovarian cancer is around 23% to 54%, which is 23-54 times the risk for the average woman.
People with these conditions should check their genetic background and consider genetic mutation testing to detect risks early.
03. Early screening for these 4 cancers is truly effective!
The low cure rate for cancer is actually closely related to the timing of detection and intervention. The World Health Organization states that cancer is preventable and treatable, and early screening and timely treatment can also lead to a high cure rate. However, it should be noted that different cancers require different screening methods, and high-risk groups can choose different screening options for early detection. For example, current clinical methods have relatively high detection rates for lung cancer, breast cancer, cervical cancer, and colorectal cancer.
Early screening can be performed using the following methods:
1) Low-dose spiral CT
Low-dose spiral CT is the preferred method for early lung cancer screening. It is simple, easy to perform, and highly sensitive to tumors. It is the primary method for early lung cancer screening, not only detecting small nodules but also promptly reflecting the morphology and location of the tumor. Regular low-dose spiral CT screening is recommended for high-risk groups, especially those over 50 years old.

2) HPV Testing and TCT Testing
Currently, the main methods for cervical cancer screening include cervical cytology (TCT) and human papillomavirus (HPV) nucleic acid testing. Women aged 25 to 64 are recommended to undergo HPV nucleic acid testing or HPV testing combined with cytology every five years; cervical cytology is recommended every three years. Women over 65 who have had normal screening results within the past 10 years and have no history of high-risk conditions do not need to undergo screening.
3) Mammography or Color Doppler Ultrasound
Breast cancer is a common malignancy with a very high global incidence. However, like all cancers, the earlier it is detected, the higher the cure rate, so early detection is crucial. Mammography and color doppler ultrasound are commonly used for early breast cancer screening, and women can begin regular screening at age 30.
4) Colonoscopy
Colonoscopy is an important tool for preventing colorectal cancer. It allows direct observation of surrounding suspicious lesions, including polyps and melanomas, and is a preventative measure to prevent malignant lesions and the risk of cancer. Studies have shown that 95% of colorectal cancers are linked to a history of polyps. It takes time for polyps to develop into cancer, potentially taking 5-10 years. Therefore, many colorectal cancer cases occur after age 55. Regular colonoscopy is recommended for those over 40.

Of course, you can't rest easy after completing these screenings. Cancer prevention still requires adjustments to your daily routine. Living a healthy lifestyle and building a strong immune system are also important preventative measures.

%20--%3e%3c!DOCTYPE%20svg%20PUBLIC%20'-//W3C//DTD%20SVG%201.1//EN'%20'http://www.w3.org/Graphics/SVG/1.1/DTD/svg11.dtd'%3e%3csvg%20version='1.1'%20id='图层_1'%20xmlns='http://www.w3.org/2000/svg'%20xmlns:xlink='http://www.w3.org/1999/xlink'%20x='0px'%20y='0px'%20width='256px'%20height='256px'%20viewBox='0%200%20256%20256'%20enable-background='new%200%200%20256%20256'%20xml:space='preserve'%3e%3cpath%20fill='%23FFFFFF'%20d='M194.597,24.009h35.292l-77.094,88.082l90.697,119.881h-71.021l-55.607-72.668L53.229,232.01H17.92%20l82.469-94.227L13.349,24.009h72.813l50.286,66.45l58.148-66.469V24.009z%20M182.217,210.889h19.566L75.538,44.014H54.583%20L182.217,210.889z'/%3e%3c/svg%3e)




